92 Sneha Nadipi
3rd Semester
Under the guidance of Dr.Roshini Reddy(intern) and Dr.Vaishnavi(PG)
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
🖌This is an ongoing case. This blog post will be updated regularly.
*️⃣CASE SENERIO:
🌡CHIEF COMPLAINTS:
📌Epigastric pain since 4 days
📌SOB since 4 days
🌡HISTORY OF PRESENT ILLNESS
Patient was apparently a symptomatic four days back then he developed
Epigastric pain and SOB since 4 days.
📌Lower limb swelling since 4 days
📌 C/O Fever, C/O cough with sputum since 4 days
📌 C/O Burning micturation
📌 C/O decreased urine output since four days
📌C/O Constipation since four days
No h/o palpitations
No h/o of chest pain
No diurnal variation
🌡PAST HISTORY
📌k/c/o CKD And patient is on conservative treatment for the same.
📌K/c/o HTN (since 6months) and is on irregular medication for same.
📌Not a known case of DM/TB/Asthma/Epilepsy/CAD/CVA/Thyroid disorders.
🌡 TREATMENT HISTORY :
📌Irregular medication for HTN since one year
📌The patient was diagnosed with CKD four years ago and is on irregular treatment since then.
📌The patients was given medication for TB 20 years ago(no clear history)
🌡PERSONAL HISTORY :
- Married
-Non-vegetarian
- Apettite loss:Yes
- Bowels : Constipation
- Micturition : Decresed Urine output and burning micturition
- No H/O known drug allergies
Addictions:
-Alcohol : regular (stopped 3 years ago)
Smoking:Chronic chutta smoker 4-5 per day (stopped 4 years ago)
🌡FAMILY HISTORY
📌Insignificant
🌡PHYSICAL EXAMINATION :
A) GENERAL EXAMINATION :
Patient is consious,coherent and cooperative,moderately built and moderately nourished
Pallor- YES
lcterus-NO
Cyanosis-No.
Clubbing of fingers/toes- No
Lymphadenopathy-No
Oedema of feet- YES
Malnutrition - Moderately nourished
Built-Moderately built
Dehydration -NO
No H/O, cyanosis , lymphadenopathy , clubbing of fingers or toes , dehydration
🌡SYSTEMIC EXAMINATION:
B) CVS
- Thrills : No
- Cardiac sounds - S1 , S2 heard
- Cardiac murmurs : No
C) RS
- BAE-PRESENT
- Dyspnea : NO
- Wheeze :Expiratory wheeze present
-Inspiratory crepts-B/L IAA ,ISA
D) ABDOMEN
- Distended
E)CNS:-Normal
1. Higher Mental Function:-
- Alert and conscious
- Normal speech
2. Cranial nerves -
- gag reflex
- vulva position
3. Motor system - attitude -
Rt. Lt.
•Reflexes. B + +
T + +
S + +
K + +
A + +
Plantars-flexors
🌡SEROLOGICAL INVESTIGATIONS:
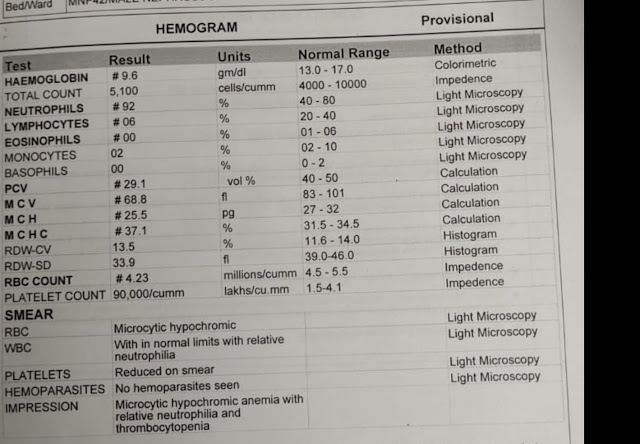
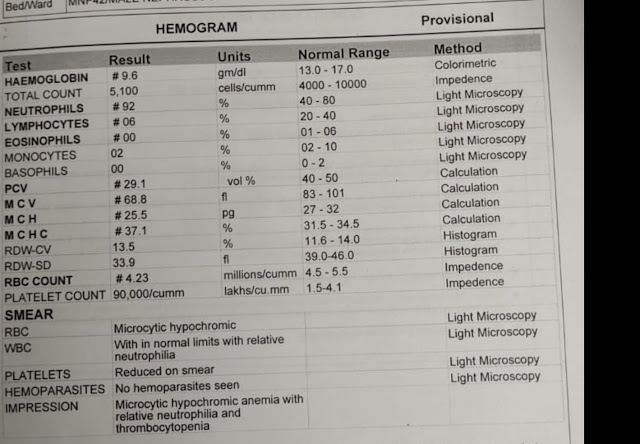
Hb-9.8 g/dl
TLC-5170 cumm
PLT(plateletcount)-43,000 cumm
Serum creatinine: 9 mg/ dl
Blood urea: 126 mg/dl
16/8/21
Serum Iron
, '

LFT.

17/8/21:
Blood urea: 238 mg/ dl
Calcium:9.9 mg/dl
Sodium : 129mEq/L
potassium : 3.5 mEq/L
chloride : 93 mEq/l
ABG
pH:7.20
Co2–24.6 mmHg
HCO3 -11.6 mEq/mol
Liver Function Test:
TB -1.08 mg/dl
DB -0.18 mg/dl
AST -31 IU/lit
ALT -88 IU/lit
Alkaline Phosphate-345 IU/lit
TP:6.2 g/dl
Alb-3.5 g/dl
A/G-1.30 g/dl
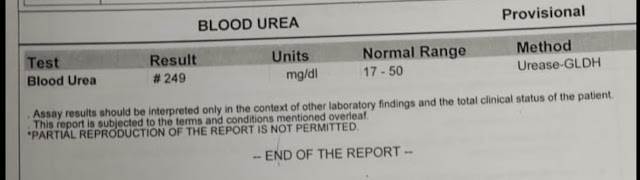
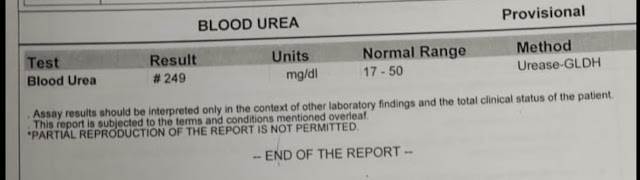
BLOOD UREA
Serum Creatinine
18/4/21
Electrolytes:
Na-124 mmol/lit
K-3.6 mmol/lit
Cl-86 mmol/lit
Hb-10.8 g/dl
TLC-4990 /cumm
PLT-50,000 /cumm
PT-16 seconds
INR-1.11
Blood Urea-145 mg/dl
Creatinine-6.7 mg/dl
Uric Acid-7.9 mg/dl
Calcium-7 mg/dl
ECG
Hemogram
ABG
RFT
At 10:27 AM
At 11:44 PM
Bacterial culture and sensitivity report

CBP
APTT
Prothrombin Time
19/8/21
Urea -167 mg/dl
Creatinine-5.8 mg/dl
Calcium-7 mg/dl
Phosphate-2.2 mg/dl
Electrolytes:
Na-126 mmol/lit
K-2.9 mmol/lit
Cl-88 mmol/lit
Hb-10.5 g/dl
TLC-6,200 /cumm
PLT-40,000 /cumm
ABG
RFT

PROVISIONAL DIAGNOSIS:
CRF
?VIRAL THROMBOCYTOPENIA
?COPD
K/C/O HTN
Treatment
16/08/21
1. Inj Lasix 40mg/IV/TID (If SBP ≥ 110 mm of hg)
2. T Nodosin 500mg/PO/TID
3. T Shelcal 500mg/PO/OD
4. T Oeofer-XT/PO/BD
5. T Amlong 5mg/PO/OD
6. Monitor vitals 4th hourly
7. Strict I/O charting
8. GRBS 8th hourly
9. Neb Duolin - 8th hourly
Budecort - 12th hourly
17/08/21
1. Inj Lasix 40mg/IV/BD
2. Tab NODOSIS 500mg/PO/TID
3. Tab Shelcal 500mg/PO/OD
4. Tab orofex-XT
5. Tab Amlung 5mg/PO/BDL
18/08/21
1. T NORDOSIS 500mg/PO/TID
2. T Shelcal 500mg/PO/OD
3. T Orofer - XT
4. T Amlong 5mg/PO/OD
19/08/21
Inj LASIX 40mg IV
Inj PAN 40mg IV
Inj CEPRAXONE 1gm IV
Tab NODOSIS 500mg P/O TID
Tab OROPER-XT P/O BD
Tab AMLONG 500mg P/O OD
Tab SHELCAL 500mg P/O OD
NEB -IPRANENT-8th hrly
-BUDUCART-12th hrly
FLUID LESLNELM <1.5 or 1 per day
Discharge Summary
🌡CHIEF COMPLAINTS:
📌Epigastric pain since 4 days
📌Lower limb swelling since 4 days
📌SOB since 4 days
📌Fever cough with sputum since 4 days
📌Burning micturation and decreased urine output since four days
📌Constipation since four days
🌡HISTORY OF PRESENT ILLNESS
Patient was apparently a symptomatic four days back then he developed
Epigastric pain and SOB since 4 days.
📌Lower limb swelling since 4 days
📌 C/O Fever, C/O cough with sputum since 4 days
📌 C/O Burning micturation
📌 C/O decreased urine output since four days
📌C/O Constipation since four days
No h/o palpitations
No h/o of chest pain
No diurnal variation
🌡PAST HISTORY
📌k/c/o CKD And patient is on conservative treatment for the same.
📌K/c/o HTN (since 6months) and is on irregular medication for same.
📌Not a known case of DM/TB/Asthma/Epilepsy/CAD/CVA/Thyroid disorders.
🌡 TREATMENT HISTORY :
📌Irregular medication for HTN since one year
📌The patient was diagnosed with CKD four years ago and is on irregular treatment since then.
📌The patients was given medication for TB 20 years ago(no clear history)
🌡PERSONAL HISTORY :
- Married
-Non-vegetarian
- Apettite loss:Yes
- Bowels : Constipation
- Micturition : Decresed Urine output and burning micturition
- No H/O known drug allergies
Addictions:
-Alcohol : regular (stopped 3 years ago)
Smoking:Chronic chutta smoker 4-5 per day (stopped 4 years ago)
🌡FAMILY HISTORY
📌Insignificant
🌡PHYSICAL EXAMINATION :
A) GENERAL EXAMINATION :
Patients is k/c/o Moderately built and Malnourished
Pallor- YES
lcterus-NO
Cyanosis-No.
Clubbing of fingers/toes- No
Lymphadenopathy-No
Oedema of feet- YES
Malnutrition - Moderately nourished
Built-Moderately built
Dehydration -NO
No H/O, cyanosis , lymphadenopathy , clubbing of fingers or toes , dehydration
🌡SYSTEMIC EXAMINATION:
B) CVS
- Thrills : No
- Cardiac sounds - S1 , S2 heard
- Cardiac murmurs : No
C) RS
- BAE-PRESENT
- Dyspnea : NO
- Wheeze :Expiratory wheeze present
-Inspiratory crepts-B/L IAA ,ISA
D) ABDOMEN
- Distended
E)CNS:-Normal
1. Higher Mental Function:-
- Alert and conscious
- Normal speech
2. Cranial nerves -
- gag reflex
- vulva position
3. Motor system - attitude -
Rt. Lt.
•Reflexes. B + +
T + +
S + +
K + +
A + +
Plantars-flexors
PROVISIONAL DIAGNOSIS:
CRF
?VIRAL THROMBOCYTOPENIA
?COPD
K/C/O HTN
SOAP NOTES
Day -1
16/8/21
Subjective
C/O
Epigastric pain
Lower limb swelling
SOB
Fever cough with sputum
Burning micturation and decreased urine output
Constipation
Objective:
Temperature
8 pm - 98.61
10 pm- 97.61
12 am - 98.61
2 am - 97.61
4 pm - 98.61
6 am - 97.62
pulse rate
8 pm - 85:
10 pm - 84
12 am - 89
4am - 84
6 am - 84
RR
8 pm - 20
10pm - 20
12 am - 18
2 am - 20
4 am - 18
6 am - 20
Spo2 (%)
8 pm - 98
10 pm - 97
12 am - 98
2 am - 97
4 am - 98
6 am - 98
BP
8 pm - 130/70
12 am - 130/70
2 am - 110/80
4 am - 110/80
6 am - 120/80
Assessment :-
Epigastric pain
SOB
Thrombocytopenia
Plan of care:-
1. Inj Lasix 40mg/IV/TID (If SBP ≥ 110 mm of hg)
2. T Nodosin 500mg/PO/TID
3. T Shelcal 500mg/PO/OD
4. T Oeofer-XT/PO/BD
5. T Amlong 5mg/PO/OD
6. Monitor vitals 4th hourly
7. Strict I/O charting
8. GRBS 8th hourly
9. Neb Duolin - 8th hourly
Budecort - 12th hourly
Day -2
17/08/21
Subjective
C/O
Epigastric pain
Lower limb swelling
SOB
Fever cough with sputum
Burning micturation and decreased urine output
Constipation
Objective:-
Tempature ( °F)
8 am - 98.61
10 am - 98.6
12 pm - 98.6
2 pm - 99.6
4 pm - 99.6
6pm - 99.6
8 pm - 98.6
Pulse rate
8 pm - 84
10 am - 88
12 pm - 84
2pm - 84
4 pm - 88
6 pm - 84
8 pm - 82
RR
8 am - 20
10 am - 18
12 pm - 18
2 pm - 20
4 pm - 20
6 pm - 21
8 pm - 19
Spo2 (%)
8am - 98
10 am - 92
12 pm - 92
2 pm - 93
4 pm - 92
6 pm - 93
8 pm - 94
BP
8 am - 120/80
10 am - 110/70
12 pm - 110/70
2pm - 110/80
4 pm - 130/70
6 pm - 120/80
8 pm - 120/70
Assessment :
Epigastric pain
SOB
Chronic Renal Failure
Known case of hypertension
COPD
Plan of care:-
1. Inj Lasix 40mg/IV/BD
2. Tab NODOSIS 500mg/PO/TID
3. Tab Shelcal 500mg/PO/OD
4. Tab orofex-XT
5. Tab Amlung 5mg/PO/BDL
Day -3
18/08/21
Subjective-
C/O
Lower limb swelling
Fever cough with sputum
Burning micturation and decreased urine output
Constipation
Decreased Epigastric pain
Objective:-
BP:120/70 mmHg
PR-142 bpm-regular
Spo2 -98% at room temperature
RR-35 cpm
Assessment :-
Decreased Epigastric pain
Decreased SOB
Chronic Renal Failure
Viral thrombocytopenia (current PLT-1 lakh cumm)
COPD
Known case of HTN
Plan of care:-
1. T NORDOSIS 500mg/PO/TID
2. T Shelcal 500mg/PO/OD
3. T Orofer - XT
4. T Amlong 5mg/PO/OD
Day -4
19/08/21
Subjective-
C/O
Decreased Epigastric pain
Lower limb swelling
Fever cough with sputum
Burning micturation and decreased urine output
Constipation
Decreased SOB
Objective:-
Temperature °F
1 am - 98.6
2am - 98.6
4 am - 98.7
6 am - 98.6
8 am - 98.6
Pulse rate
1 am - 82
2 am - 86
4 am - 84
6 am -86
8 am - 82
RR
1am - 19
2 am - 22
4 am - 26
6 am - 26
8 am - 24
Spo2
1 am - 96
2 am - 98
4 am - 98
6 am - 98
8 am - 99
BP
1 am - 120/80
2 am - 120/80
4 am - 120/80
6 am - 120/80
8 am - 120/80
Assessment :
Decreased Epigastric pain
Decreased SOB
CRF
Viral thrombocytopenia
COPD
Known case of HTN
Past h/o of pulmonary Koch
Hyponatremia (hypervolemia 2 to CRF)
Hypocalcemia
Plan of care:-
Inj LASIX 40mg IV
Inj PAN 40mg IV
Inj CEPRAXONE 1gm IV
Tab NODOSIS 500mg P/O TID
Tab OROPER-XT P/O BD
Tab AMLONG 500mg P/O OD
Tab SHELCAL 500mg P/O OD
NEB -IPRANENT-8th hrly
-BUDUCART-12th hrly
FLUID LESLNELM <1.5 or 1 per day
FEVER CHART(16/08-19/08)
Treatment
16/08/21
1. Inj Lasix 40mg/IV/TID (If SBP ≥ 110 mm of hg)
2. T Nodosin 500mg/PO/TID
3. T Shelcal 500mg/PO/OD
4. T Oeofer-XT/PO/BD
5. T Amlong 5mg/PO/OD
6. Monitor vitals 4th hourly
7. Strict I/O charting
8. GRBS 8th hourly
9. Neb Duolin - 8th hourly
Budecort - 12th hourly
17/08/21
1. Inj Lasix 40mg/IV/BD
2. Tab NODOSIS 500mg/PO/TID
3. Tab Shelcal 500mg/PO/OD
4. Tab orofex-XT
5. Tab Amlung 5mg/PO/BDL
18/08/21
1. T NORDOSIS 500mg/PO/TID
2. T Shelcal 500mg/PO/OD
3. T Orofer - XT
4. T Amlong 5mg/PO/OD
19/08/21
Inj LASIX 40mg IV
Inj PAN 40mg IV
Inj CEPRAXONE 1gm IV
Tab NODOSIS 500mg P/O TID
Tab OROPER-XT P/O BD
Tab AMLONG 500mg P/O OD
Tab SHELCAL 500mg P/O OD
NEB -IPRANENT-8th hrly
-BUDUCART-12th hrly
FLUID LESLNELM <1.5 or 1 per day
















Comments
Post a Comment